Big Changes Are Coming To Cervical Screenings That Will Affect Millions Of Women
The NHS announced this earlier this week, backed by significant clinical evidence.

Health guidelines evolve as research uncovers better ways to protect people without adding unnecessary steps. One area where this is currently happening is cervical screening. The NHS has just announced a major update to how often people are invited to get screened, and if you're eligible, this will likely affect you.
So, what is cervical screening, and why should you care? Cervical screening is a test designed to help prevent cervical cancer.
It checks for high-risk types of HPV (human papillomavirus), which can cause changes in the cells of the cervix. If left unchecked, these cell changes can sometimes develop into cancer. If HPV is detected during screening, the sample is also tested for any abnormal cervical cells.
The test is offered to women and anyone with a cervix between the ages of 25 and 64. Until now, people under 50 were invited for screening every three years, assuming their last result was clear.
From age 50 to 64, the interval increased to every five years. That has been the process for a while. But starting this week (10 June), things are shifting.
The NHS will now invite people for screening every five years, regardless of whether they are under or over 50, as long as their last test showed no cause for concern.
The NHS has just revealed a significant update to cervical screening in England.
This isn’t just a random change. It’s based on research and evidence. A pilot study led by researchers at King’s College London, published in the BMJ in 2022, found that switching to five-year intervals after a negative HPV test is just as safe as sticking to the three-year schedule.
The key point? The same number of cancers were detected, just with fewer tests. In short, if your HPV test comes back negative, you’re considered at very low risk of developing cervical cancer in the short term. That means testing more often doesn’t make a meaningful difference.
Dr. Sue Mann, NHS National Clinical Director for Women’s Health, explained the logic behind the update:
 unsplash
unsplashThe NHS explains the rollout of more tailored cervical screening for millions.
England is catching up to the rest of the UK with this decision. Scotland and Wales already follow the five-year interval, based on recommendations from the UK National Screening Committee (UKNSC). Now, England is aligning with the same evidence-based guidance.
Michelle Mitchell, Chief Executive of Cancer Research UK, also weighed in:
“We welcome this change to cervical screening in England, which is the result of years of vital research to make screening more effective and has shown it is safe to extend the time between tests.”She also pointed out how far we've come in tackling cervical cancer.
“Screening, alongside the rollout of the HPV vaccine, which Cancer Research UK scientists helped develop, has seen cervical cancer rates drop by around a quarter since the early 1990s.”And while the new approach will reduce the number of appointments people need, Mitchell reminded everyone not to ignore warning signs.
“If you notice any unusual changes, do not wait for a screening invitation – speak to your doctor.”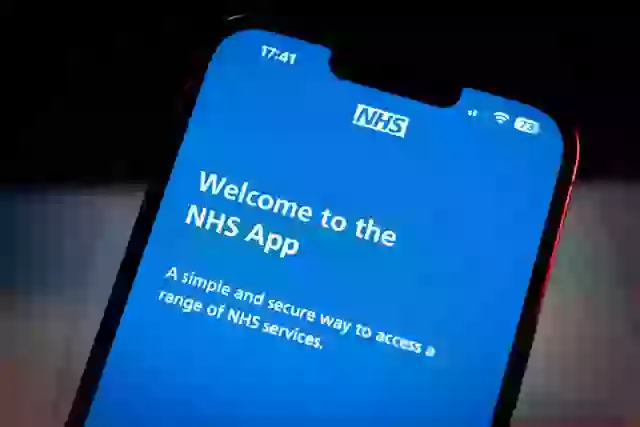 Getty Images
Getty Images
For some, less frequent screenings may come as a relief. According to Healthwatch England, many women find the experience physically uncomfortable and hard to schedule around work, childcare, and other commitments.
Louise Ansari, Chief Executive of the organization, said:
“Reducing the number of times they need to attend, alongside sensitive and empathetic approaches by health professionals, will make these important appointments easier to manage.”The bottom line? If your results are clear, five years between screenings is now the new normal. It’s not about cutting corners; it’s about doing what works best based on solid evidence.
And if anything feels off between screenings, it’s still important to speak up. The system may be evolving, but the goal remains the same: keeping people safe.
Evolving Guidelines for Cervical Screening
Dr. Jennifer Gunter, an obstetrician and gynecologist, emphasizes that the NHS's new cervical screening guidelines reflect a growing understanding of HPV's role in cervical cancer prevention. By extending intervals between screenings, the NHS aims to balance patient comfort with effective cancer prevention.
She notes, “This approach not only reduces the burden on healthcare systems but also aligns with evidence suggesting that more frequent screenings do not significantly enhance outcomes.” Gunter's insights underscore the importance of adapting healthcare practices based on emerging research.
Dr. Lila N. Hurst, a public health researcher, advises that women should actively engage with their healthcare providers regarding these new cervical screening recommendations. She suggests asking questions like, 'How will this change affect my individual risk factors?' and 'What should I expect during this transition?' Such proactive communication can help personalize care.
Furthermore, Dr. Hurst emphasizes the importance of maintaining regular check-ups and discussing any concerns with healthcare professionals, as personal history and family background can significantly influence screening needs.
Solutions & Coping Strategies
The recent updates to cervical screening guidelines by the NHS are a significant step forward, driven by clinical evidence and expert insights. As research shows, adapting health practices in response to new findings is crucial for enhancing patient care. Women should feel empowered to communicate openly with their healthcare providers about their individual risks and screening schedules.
Ultimately, fostering an environment of understanding and support can lead to better health outcomes, ensuring that women remain informed and proactive in their healthcare journeys.