Experts Weigh In on CDC's Decision to Discontinue Hepatitis B Vaccines for Newborns - Heartfelt Reactions Shared
CDC's Shift in Hepatitis B Vaccine Policy Stirs Controversy Among Health Professionals.

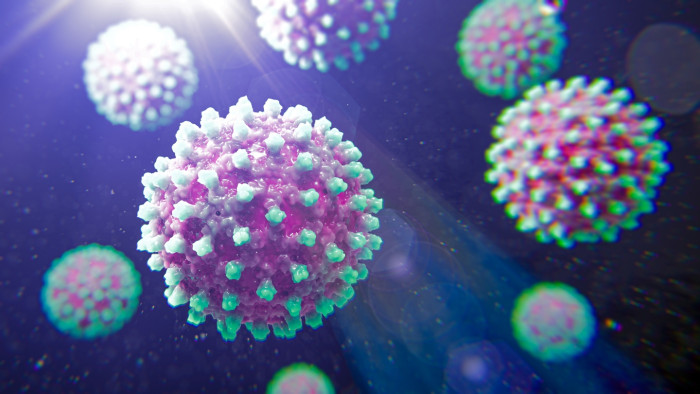
The recent decision by the Centers for Disease Control and Prevention (CDC) to discontinue the administration of hepatitis B vaccines to newborns has stirred a heated discussion among healthcare professionals and experts. Influenced by recommendations from the CDC's Advisory Committee on Immunization Practices (ACIP), the new guidelines propose delaying the hepatitis B vaccine for infants born to virus-negative mothers until they are two months old.
This shift in policy represents a significant departure from the longstanding practice of administering the vaccine shortly after birth. The CDC's announcement opens the door for parents to make personalized choices regarding their newborns' vaccination, especially in cases where the mother tests negative for hepatitis B.

CDC's Revised Hepatitis B Vaccine Guidelines Spark Controversy
The CDC's decision to revise the guidelines for administering hepatitis B vaccines to newborns has raised concerns among healthcare professionals and parents alike. This shift in policy emphasizes the importance of personalized healthcare choices, particularly for infants born to virus-negative mothers.
While the new recommendations aim to provide more flexibility in vaccination schedules, they have also sparked discussions about the potential impact on public health strategies.
CDC Adopts New Approach to Prevent Hepatitis B Transmission
According to the CDC, the decision to adopt this new approach was made in light of a thorough review of the existing evidence surrounding the risks of hepatitis B transmission from mother to child. In a press release detailing the change, the CDC stated: "The Centers for Disease Control and Prevention (CDC) today adopted individual-based decision-making for hepatitis B immunization for parents deciding whether to give the hepatitis B vaccine, including the birth dose, to infants born to women who test negative for the virus.
For those infants not receiving the birth dose, it is suggested that the initial dose be administered no earlier than two months of age." This statement underscores the CDC's emphasis on informed consent and parental choice in the context of vaccination. Hepatitis B is a viral infection that primarily affects the liver and is transmitted through contact with infectious body fluids, including blood.
Consequences of Untreated Hepatitis B Infections
The virus can lead to chronic liver disease, cirrhosis, and even liver cancer if left untreated. The National Health Service (NHS) outlines several ways in which hepatitis B can be contracted, including through sexual contact, sharing needles, and from mother to child during childbirth.
Most individuals infected with hepatitis B may not exhibit symptoms, or they may experience only mild symptoms, which can make the disease particularly insidious. The decision to alter the vaccination protocol has drawn criticism from various medical professionals.
Jim O'Neill on CDC's Vaccination Recommendation for Newborns
Jim O'Neill, the Acting Director of the CDC and Deputy Secretary of Health and Human Services, commented on the decision, stating, “This recommendation reflects ACIP’s rigorous review of the available evidence. We are restoring the balance of informed consent to parents whose newborns face little risk of contracting hepatitis B.” While O'Neill's remarks suggest a focus on parental autonomy, many experts worry that this change could lead to increased vulnerability among infants who may be at risk of hepatitis B infection.
The hepatitis B vaccination program for newborns was first introduced in 1991, and since then, it has played a crucial role in reducing the incidence of the disease among children. Experts from the Children's Hospital of Philadelphia have noted that this immunization initiative has led to the disease being "virtually eliminated" in the pediatric population.
Breakthrough: Vaccine Success in Preventing Hepatitis B Transmission
This remarkable achievement has been attributed to the widespread adoption of the vaccine, which has proven effective in preventing the transmission of hepatitis B from mothers to their infants. Kressly, the president of the American Academy of Pediatrics (AAP), expressed her dismay at the CDC's decision, describing it as "heartbreaking." She stated, “As a pediatrician, this is heartbreaking when we have a vaccine that can prevent so many infections, and it is deeply disappointing to see the continued dismissal of expertise to inform recommendations that have broad implications on the health of America's children." Dr.
Kressly's comments highlight the concerns of many healthcare professionals who fear that delaying the vaccine could result in preventable infections and complications among vulnerable infants. The implications of this decision extend beyond individual health choices; they also raise questions about public health policy and the role of vaccination in disease prevention.
The Importance of Hepatitis B Vaccination
Vaccines have historically been one of the most effective tools in controlling infectious diseases, and the hepatitis B vaccine is no exception. The World Health Organization (WHO) has long advocated for the inclusion of the hepatitis B vaccine in national immunization programs, particularly in regions where the virus is endemic.
In light of the CDC's new recommendations, parents who wish to have their newborns vaccinated against hepatitis B at birth are encouraged to consult with their healthcare providers. This conversation is crucial, as healthcare professionals can provide personalized guidance based on the family’s medical history and the potential risks associated with hepatitis B.
The Importance of Timely Hepatitis B Vaccination for Children
It is essential for parents to understand the importance of timely vaccination, especially considering the potential long-term health consequences of hepatitis B infection. Moreover, the decision to delay vaccination could have broader implications for public health.
Experts warn that if a significant number of parents choose to postpone or forgo the hepatitis B vaccine for their newborns, it could lead to an increase in hepatitis B cases in the community. This is particularly concerning in light of the fact that hepatitis B can be transmitted from mother to child during childbirth, and infants are at a higher risk of developing chronic infections if they contract the virus early in life.
Parental Choice in Vaccination: The Growing Trend
The CDC's decision also reflects a growing trend in public health discussions surrounding vaccination and parental choice. In recent years, there has been an increasing emphasis on informed consent and the right of parents to make healthcare decisions for their children.
While this approach is rooted in respect for individual autonomy, it also raises important questions about the balance between personal choice and community health. Public health experts argue that vaccination is not only a personal decision but also a collective responsibility, as high vaccination rates are essential for herd immunity and the protection of vulnerable populations.

Navigating Vaccination Decisions: Parental Awareness and Informed Choices
As the debate continues, it is crucial for parents to remain informed about the risks and benefits of vaccination. Engaging in open discussions with healthcare providers can help parents make well-informed decisions that prioritize their child's health while also considering the broader implications for public health.
Vaccination is a critical component of preventive healthcare, and understanding its importance can empower parents to make choices that protect not only their children but also the community at large. In conclusion, the CDC's recent decision to allow for the delayed administration of the hepatitis B vaccine for newborns born to mothers who test negative for the virus has ignited a complex discussion about vaccination policies and parental choice.
Balancing Informed Consent and Vaccine Risks for Parents
While the intention behind the change may be to promote informed consent, it is essential to consider the potential risks associated with delaying vaccination. As experts continue to weigh in on this issue, it is vital for parents to engage with healthcare professionals to ensure that they are making informed decisions that safeguard their children's health and contribute to the overall well-being of the community.
The importance of vaccination in preventing infectious diseases cannot be overstated, and ongoing dialogue about these policies will be crucial in shaping the future of public health initiatives.