Survivor Describes Living Beyond Her Body During a Three-Week Coma
The woman described dreams that felt even more real than waking life.
Sometimes life throws us into situations we never expect, testing both our bodies and minds in ways that feel unreal. One moment you’re fine, and the next, everything changes, often without warning.
This is what happened to Amanda van der Gulik, a Canadian YouTuber who recently shared a terrifying experience that turned her life upside down. What started as what seemed like a common cold quickly spiraled into a fight for survival and a strange journey through vivid, almost otherworldly dreams while she was in a coma.
Amanda’s story began when she caught what she thought was just a bad cold. However, the illness didn’t improve.
It got worse. She says doctors initially thought she had pneumonia but didn’t fully grasp how serious it was.
“They thought it was just a bad cold,” Amanda explained.
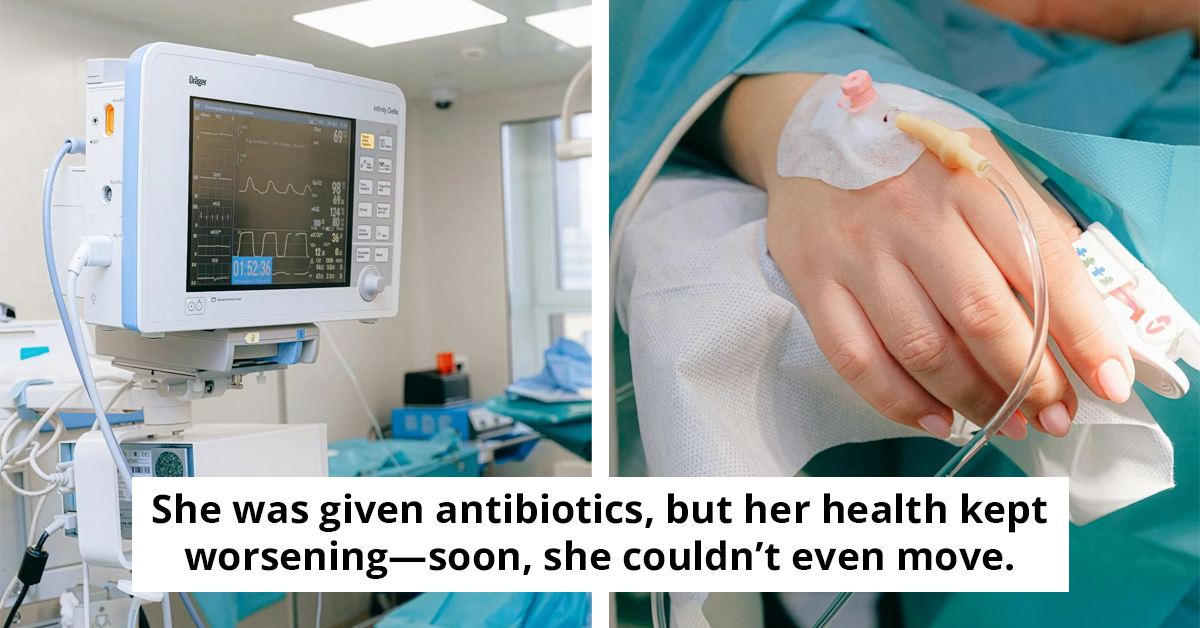
She was prescribed antibiotics, but her condition continued to decline. Eventually, she reached a point where she couldn’t even move.
Realizing something was seriously wrong, Amanda and her partner returned to the hospital, this time to the emergency room. That’s when things took a grim turn.
Tests showed that the infection had spread to both of her lungs, her oxygen levels had dropped dangerously low, and she needed urgent care. Unfortunately, the hospital where they were didn’t have an intensive care unit (ICU), so the doctors said she needed to be transferred to another hospital that did.
Amanda said doctors didn’t realize at first that she had pneumonia.
The nearest ICU was 45 minutes away. However, to move Amanda safely, the doctors had to put her into a medically induced coma. The plan was straightforward: she would remain in the coma for a few days, just enough time to stabilize her condition, then they’d take her off sedation and start her recovery.
But things didn’t go as planned. Amanda’s health didn’t improve. Instead, it worsened. She developed something called acute respiratory distress syndrome, or ARDS, which meant her lungs stopped functioning correctly.
Amanda described it bluntly: “My lungs had given up and couldn’t function on their own.”This complication extended her time in the coma to three weeks. During those three weeks, Amanda says she experienced some of the most intense and frightening dreams of her life. She spoke openly about what it was like, not holding back.
 Getty Stock Image
Getty Stock ImageAmanda described vivid nightmares filled with her fears and memories.
Her mind replayed every significant moment from her life, every fear, every painful memory, and every time she’d been manipulated or hurt. All those experiences became tangled together into one terrifying horror story in her head.
“It was like I lived a second life,” Amanda said. “The memories felt stronger than my regular memories, clearer, and they haven’t faded. They’re still with me.”Hearing about this was shocking, but it’s something that happens to many people who spend time in intensive care. The brain’s way of dealing with extreme stress and sedation can create these intense, sometimes disturbing dreams that linger long after waking up.
Thankfully, after three weeks, Amanda’s lungs started functioning better, and she was able to come out of the coma. That marked the beginning of her physical recovery.
Looking back, Amanda admits the experience was terrifying, but over time, the grip those nightmares had on her mind has lessened.
“It’s still a bit there, but it’s not as bad as it was,” she said. Getty Stock Image
Getty Stock Image
Her experience shows how quickly serious illness can strike and how the challenges of critical care, including unusual mental states, can be as tough as the physical recovery itself.
By sharing her story openly, Amanda highlights the harsh realities many ICU patients face and the incredible strength needed to overcome them.
Understanding Coma Experiences
Dr. Sam Parnia, a critical care physician and researcher, highlights that experiences during coma can vary widely among individuals. According to his studies, many patients report vivid dreams or out-of-body experiences, suggesting a complex interplay between brain activity and consciousness.
Parnia emphasizes the importance of understanding these phenomena, as they can significantly affect recovery. He advocates for integrating psychological support into medical recovery plans, allowing individuals to process their experiences and emotions related to their coma and subsequent awakening.
Experts in trauma, like Dr. Tara Brach, suggest that integrating mindful practices can help individuals who have experienced trauma, such as a coma. Mindfulness can foster emotional healing through increased self-awareness and acceptance of one's experiences.
Additionally, Brach recommends techniques like meditation and breathing exercises to help patients manage anxiety or confusion post-recovery. These practices can facilitate emotional resilience, enabling individuals to ground themselves and navigate their feelings, ultimately leading to a more holistic recovery process.
Research-Based Understanding
Insights from healthcare professionals indicate that experiences during comas can offer profound insights into consciousness and recovery. Understanding these complex interactions is crucial for tailored rehabilitation.
As Dr. Parnia notes, fostering a supportive environment with psychological resources can enhance recovery outcomes. This approach not only addresses physical healing but also the emotional and psychological aspects of trauma, as outlined by experts like Dr. Brach. Thus, integrating comprehensive care for both mind and body is essential for holistic recovery and well-being.